New Model for Classifying Types of Batten Disease Proposed
Hypothesis posits 'top-down,' 'bottom-up' view based on lipofuscin accumulation
Written by |
Researchers have proposed an alternate classification model for Batten disease types based on the site first affected by each type and how it progresses. They tested their hypothesis in two of the most common Batten types.
A comprehensive analysis of published data so far showed infantile Batten disease — an early-onset, severe, and rapidly progressing type — starts outside the brain and could represent a “bottom-up” form of Batten.
In turn, juvenile Batten disease — a later-onset and slowly progressing type — first affects the retina (the innermost, light-sensitive eye layer) then the brain and then the nerves outside the brain, potentially representing a “top-down” form.
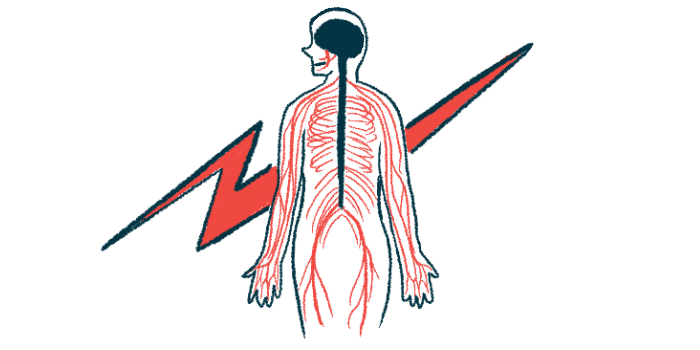
These distinct patterns of disease progression share similarities with Parkinson’s disease, whereby loss of nerve cells can either start in the brain then spread to other parts of the nervous system (“brain-first”) or begin in the nerves then spread to the brain (“body-first”).
The proposed model was detailed in the study “Top-down and bottom-up propagation of disease in the neuronal ceroid lipofuscinoses,” published in Frontiers in Neurology.
Batten disease, also called neuronal ceroid lipofuscinoses (NCLs), is a group of inherited neurological conditions marked by the accumulation of lipofuscin, a mixture of proteins and fatty molecules. Brain cells are particularly susceptible to the harmful effects of excess lipofuscin, but eyes, skin, and muscles can also be affected.
The condition is caused by variants in 13 different genes and is classified into five types based on the age of onset and severity of symptoms: congenital, infantile, late infantile, juvenile, and adult.
Distinguishing NCLs by where lipofuscin accumulates
While NCLs can be considered distinct disorders with separate underlying molecular and genetic causes, researchers in the U.S., the U.K., and Denmark proposed an alternative way to understand and classify the different types of the disorder.
They hypothesized that Batten types can be considered as related neurodegenerative diseases, all caused by toxic lipofuscin accumulation, but distinguished by where the disease first appears in the body and how it progresses.
The team compared the clinical characteristics, imaging data, and postmortem or autopsy findings of people with infantile and juvenile Batten — two of the most common forms.
Infantile Batten, also known as CLN1 disease, is a very early-onset, severe, and rapidly progressive type caused by mutations in the PPT1 gene. Juvenile Batten, the most common type, is a later-onset, slowly progressive form caused by CLN3 gene mutations.
The data analyses showed that in CLN1 disease, lipofuscin deposits have been reported in some intestinal nerves and those of the autonomic system as early as three months, before any signs of symptoms. The autonomic nervous system controls involuntary bodily functions such as heartbeat, blood flow, and digestion.
These deposits are also present in the nerves lining the gut and supplying the internal organs, as well as in the skin.
Brain manifestations appeared at the end of the first year, with generalized and increasing atrophy of all brain regions. Atrophy is also seen in movement-involved muscles, where relatively little lipofuscin is detected.
Mental development begins to slow around one year, followed by motor decline, irritability, and disturbed sleep. By age 3, alongside widespread brain and eventual retinal involvement, the disease reaches a so-called “burnt-out” stage with little electrical brain activity, unresponsive behavior, and little voluntary movement.
Seizure frequency is high at first but tends to decrease in the later stages. Children have a life expectancy of 7–12 years. Researchers refer to this type that starts in the body and spreads up to the brain as a “bottom-up” form.
In contrast, the first symptom of CLN3 disease is rapid loss of vision with impaired retinal activity detected between ages 5–7, and complete vision loss three to four years later.
Retinal involvement is followed by cognitive decline, behavior changes, and seizures. Brain atrophy is not seen until about age 9 and is strongest after age 14, but brain connectivity abnormalities are evident before age 10.
Progressive motor impairment begins in adolescence, with eventual wheelchair use needed. Unlike CLN1 disease, the frequency of seizures is initially low, but worsens moderately as the disease progresses. Most CLN3 patients are bedridden by their 20s, and typically live until their 30s.
Only in postmortem samples of juvenile Batten patients is lipofuscin seen to build up within autonomic nerve cells of the gut and in the nerves supplying the muscles. Researchers have proposed that juvenile Batten that starts in the brain and spreads to the body could be classified as a “top-down” form.
These findings highlight “a great difference in the progression of clinical symptomatology and [disease features] between two major forms of Batten disease, not only in relation to rate of disease progression, but also which parts of the … nervous system are affected first and the extent to which different regions are vulnerable to disease,” the researchers wrote.
They also noted that the juvenile-onset form of CLN1 disease, which starts between ages 5–10, also affects the brain first, leading to motor decline and seizures in the years that follow. Vision loss only occurs in early adolescence.
“This means that the occurrence of different CLN1 disease courses of infantile or juvenile nature actually fits well with the proposed hypothesis and does not contradict it,” the researchers wrote.
This new model “is of great importance when considering how to monitor treatment results during disease course most appropriately, but it also has consequences for which route of administration to choose,” they wrote, noting their “top-down” versus “bottom-up” hypothesis should be evaluated and refined and that “mechanistic studies will be needed to reveal its underlying basis not just in mouse models, but also in larger animal models.”