Use of gemfibrozil shows promise in mouse model of juvenile Batten
Fat-lowering medicine found to improve motor function in new study
Use of the cholesterol medication gemfibrozil — a fat-lowering therapy — reduced brain inflammation and improved motor function in a mouse model of juvenile Batten disease, a new study reports.
These therapeutic benefits were mediated by the activation of peroxisome proliferator-activated receptor-alpha, known as PPAR-alpha. This receptor protein regulates fat metabolism, inflammation, and oxidative stress, a type of cellular damage, in the brain.
The findings suggest that therapeutic approaches activating PPAR-alpha may lessen the progression of juvenile Batten, also called CLN3 disease.
“If these results are replicated in patients, it would open up a promising avenue of treatment of this devastating disease and stop the disease in its tracks,” Kalipada Pahan, PhD, the study’s senior author and a professor of neurology at Rush University Medical College, in Chicago, said in a press release.
The study, “Activation of PPARα Exhibits Therapeutic Efficacy in a Mouse Model of Juvenile Neuronal Ceroid Lipofuscinosis,” was published in The Journal of Neuroscience.
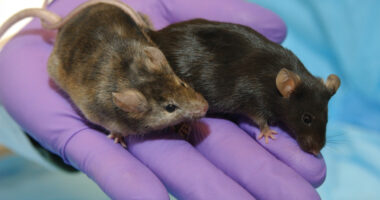
Testing the use of gemfibrozil in a CLN3 mouse model
A type of Batten disease, juvenile Batten usually results in symptoms between the ages of 5 and 10, which typically begin with motor impairments. It is caused by a mutation in the CLN3 gene, which provides the instructions to make a protein called battenin.
Lack of battenin leads to the toxic buildup of an autofluorescent fatty substance called lipofuscin inside lysosomes, the cell’s recycling centers. This ultimately kills cells, particularly nerve cells, and promotes inflammation in the brain, or neuroinflammation.
“Finding an effective drug to protect the brain and stop the progression of Batten is an important area of research,” Pahan said.
A previous study showed that gemfibrozil, an oral medication used to reduce fatty molecules in the blood, lessened disability and increased the lifespan of mice with late infantile Batten, a form of Batten with a symptom onset between 2-4 years of age.
Sold under the brand name Lopid and others, with generics available, gemfibrozil works by activating PPAR-alpha. Besides its fat-lowering properties, the therapy has been shown to have neuroprotective and anti-inflammatory effects.
Now, Pahan and colleagues at Rush University Medical Center assessed whether gemfibrozil treatment also promoted therapeutic benefits in a mouse model of juvenile Batten that harbors the most common disease-causing CLN3 mutation.
The work was supported by Polaryx Therapeutics, which is working toward treatments for CLN3 disease, and a grant from the National Institutes of Health.
The team found that gemfibrozil lessened neuroinflammation by reducing the activation of microglia cells, the brain’s resident immune cells, and astrocytes, cells involved in the provision of nutrients to neurons. Microglia and astrocyte abnormal activation has been shown to be a driver of neuroinflammation.
The therapy also eased the accumulation of autofluorescent deposits in the somatosensory cortex and improved the animals’ motor activity. The somatosensory cortex is a brain region that processes all sensory input from the body.
“We have found that oral gemfibrozil successfully reduces inflammation in the brain, decreases brain accumulation of toxic autofluorescent pigment deposits and improves locomotor activities in mice that are missing the CLN3 gene,” Pahan said.
Treated mice also showed increased levels of PPAR-alpha, which was markedly reduced in the somatosensory cortex of untreated animals.
These results suggest that activation of [PPAR-alpha] may be beneficial for [juvenile Batten] and that gemfibrozil may be repurposed for the treatment of this incurable disease.
In further analyses, gemfibrozil was found to restore the brain levels of the transcription factor EB (TFEB), a master regulator in the generation of lysosomes, by promoting PPAR-alpha’s binding to the TFEB gene, triggering its activation.
“We were excited to see that oral gemfibrozil activates TFEB in the brain, which is the beginning of the process for clearing out dead cells from the body,” Pahan said.
Genetically depleting the mouse model of PPAR-alpha worsened the animals’ health, and gemfibrozil no longer exerted its therapeutic effects. In these mice, the therapy was unable to reduce the toxic accumulation of fatty deposits, microglia and astrocyte activation, or improve motor function.
“Our mechanistic finding suggests that gemfibrozil may not be beneficial for Cln3 brain that is lacking [PPAR-alpha],” Pahan said.
“These results suggest that activation of [PPAR-alpha] may be beneficial for [juvenile Batten] and that gemfibrozil may be repurposed for the treatment of this incurable disease,” the researchers wrote.
Polaryx is planning to launch a Phase 3 clinical trial (NCT04637282) to assess the safety, tolerability, and effectiveness of multiple doses of its juvenile Batten therapy candidate, PLX-200, against a placebo. That study will involve children and adolescents, ages 6 to 18, with the rare disease.
PLX-200 is a repurposed medicine, originally developed to lower cholesterol, that binds to retinoid X receptor-alpha, a protein that activates other genes when bound by its ligand, PPAR-alpha.