Abnormal Autophagy Is Common in Lysosomal Storage Diseases, Including Batten
Written by |
A recent review highlights how autophagy, a process in the body that deals with the destruction of cells to maintain balance and normal functions, is impaired in patients with lysosomal storage disorders (LSDs) such as Batten disease, and could eventually be a therapeutic target for disease.
The study, “Dysregulation of autophagy as a common mechanism in lysosomal storage diseases,” was published in the journal Essays in Biochemistry.
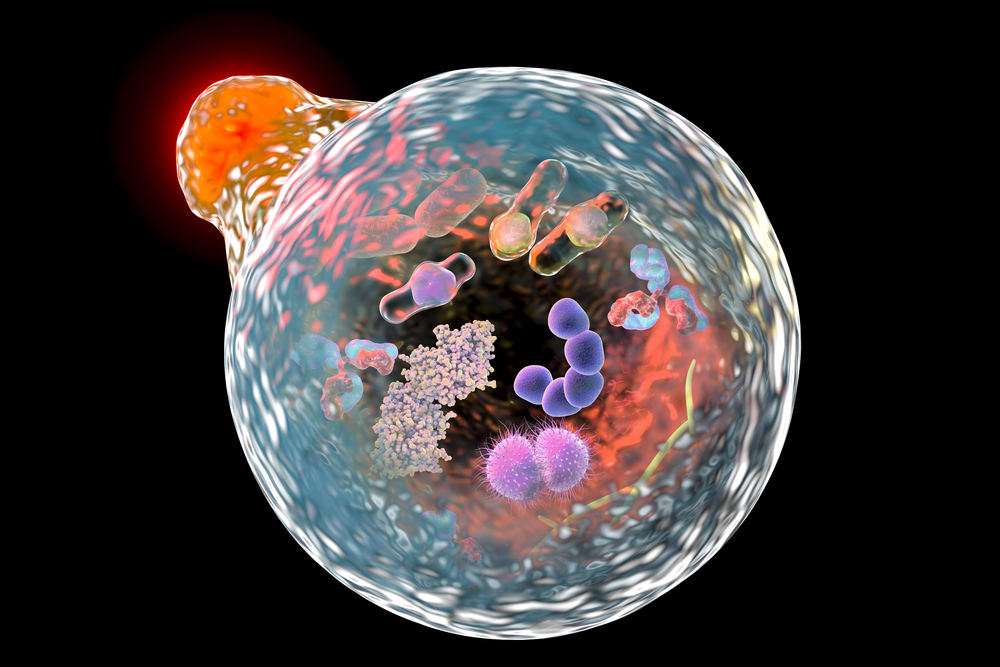
Studies have shown the lysosome is not simply a machine for the degradation of cellular components, it’s a critical mediator of cellular metabolism.
The importance of the lysosome for cellular function is seen in the large number of diseases associated with dysfunctional lysosomes, known as lysosomal storage disorders (LSDs).
Lysosomes are the terminal degradative organelles for autophagy, a key pathway to either degrade damaged or excess cell components or recycle cellular products that are commonly found to be abnormal in neuronal ceroid lipofuscinoses (NCLs).
While faulty cell death processes have been implicated in many different diseases, including cancer and various cardiovascular, metabolic, pulmonary and infectious disorders, the nervous system has been seen to be extremely susceptible.
In fact, dysregulated autophagy has been identified in almost every late-onset neurodegenerative disorder, and similar defects are now being recognized in NCLs.
Current research has implicated 13 genes that play a role in the development of NCL. Several of these genes provide instructions for lysosomal proteins, such as soluble enzymes/proteins, membrane proteins, or for endoplasmic reticulum (ER) membrane proteins, cytosolic proteins, and those expressed in the secretory pathway.
Collectively, these genes are involved in the autophagy pathway.
Several studies in NCL mouse models have indicated abnormal cell death. In fact, a recent study showed an accumulation of autophagy components coupled with lysosomal dysfunction in the brain, suggesting that a block in “autophagic flux” may be happening.
These results were similar to those seen in mouse models of two neuronal ceroid lipofuscinosis diseases, as well as in NCL patient-derived cells.
Cln3-deficient mouse modeling Batten disease has also revealed defective maturation of cell death machinery, which was associated with an increase in autophagic and lysosomal compartments.
Additionally, loss of cathepsin function, a protein commonly mutated in different NCLs, leads to dysregulated autophagy which results in neurodegeneration observed in mouse models that mimic the human disease.
Understanding more about the role of autophagy in NCLs may help determine new targets that can be used to develop future therapies. And although cell death inducers have already shown benefit in a few LSDs, a broader evaluation is urgently required.