Extracellular Vesicles May Enhance Delivery of TPP1 to the Brain for Replacement Therapy in CLN2, Early Study Suggests
Written by |
Extracellular vesicles derived from a type of immune cell called macrophage may hold potential as a less-invasive delivery system of TPP1 — the enzyme missing in patients with CLN2 or late infantile Batten disease — to the brain of affected individuals.
The preclinical study with that finding, “TPP1 Delivery to Lysosomes with Extracellular Vesicles and their Enhanced Brain Distribution in the Animal Model of Batten Disease,” was published in the journal Advanced Healthcare Materials.
Like other lysosomal storage disorders, CLN2 or late infantile Batten disease, is caused by genetic mutations that prevent cells from effectively breaking down waste material inside lysosomes, which are cell structures that digest and recycle different types of molecules.
Patients with CLN2 disease carry mutations in the TPP1 gene, leading to severe deficiency or complete lack of the TPP1 enzyme. That results in incomplete breakdown of protein fragments, known as peptides, inside lysosomes. As a consequence, toxic waste material accumulates inside cells, primarily in the nervous system, causing the signs and symptoms of CLN2 disease.
Delivering a functional TPP1 to the central nervous system (CNS, brain and spinal cord) has been considered a mainstay approach to treat the disease. In fact, it forms the basis of the only approved treatment for this condition: Brieneura (cerliponase alfa, sold by BioMarin), an enzyme replacement therapy that delivers a functional TPP1 enzyme to the brain.
However, the administration of this therapy requires invasive infusions known as intraventricular injections into the fluid of the brain.
One of the major reasons why therapeutics are not successfully delivered to the CNS using less-invasive, systemic methods — into the bloodstream, for example — is the existence of multiple biological barriers that limit effective drug delivery to the CNS, particularly the blood brain barrier (BBB), a highly selective semipermeable membrane that separates the circulating blood from the brain.
To circumvent this problem, researchers at University of North Carolina at Chapel Hill propose using extracellular vesicles (EVs) as nanocarriers for effectively delivering TPP1 to the brain, even when administered systemically (into the blood) .
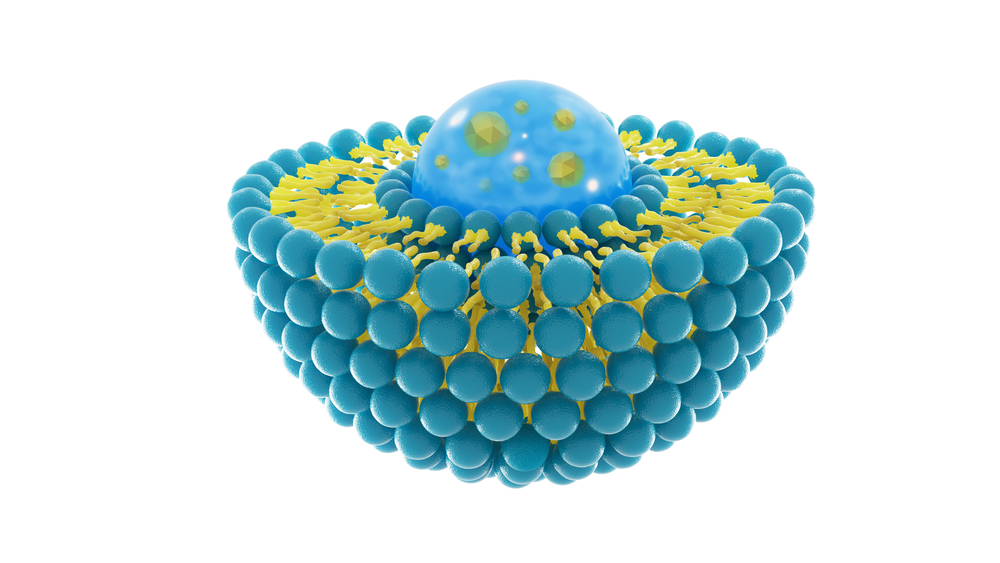
EVs are naturally occurring, microscopic, membrane-enclosed vesicles, used by cells to communicate with each other “and therefore can provide unprecedented opportunities for delivering drugs,” the researchers wrote.
EVs have been suggested as drug delivery carriers for varying purposes, including the delivery of anti-inflammatory or anti-cancer agents.
To optimize TPP1 delivery to the brain, scientists tested certain EVs that are specifically found in immune cells known as macrophages that participate in inflammatory responses. Nerve cell death is often accompanied by neuroinflammation in lysosomal storage disorders, such as Batten disease. That’s why macrophage EVs have the potential for site-specific delivery of TPP1 to brain regions affected by inflammation.
In this study, researchers generated macrophage-derived EVs loaded with TPP1 and tested if these carriers could effectively deliver the therapeutic protein to cellular and mice models of CLN2 disease.
To this end, TPP1 was loaded onto macrophage-derived EVs using two different methods: macrophages were genetically engineered to produce TPP1 and load it on EVs; or TPP1 was incorporated into empty EVs derived from macrophages.
Both methods provided efficiently incorporated functional TPP1 into EVs.
As anticipated, EVs protected TPP1 from degradation and enabled efficient transport of the functional enzyme to in vitro cell models of CLN2 (patients’ skin cells grown in petri dishes).
Most EV-TPP1 (about 70%) were confirmed to be delivered to lysosomes, the cell compartment where TPP1 enzyme is missing.
Importantly, when researchers systemically administered TPP1-loaded EVs to mouse models of Batten disease (late infantile NCL mice) there was a robust accumulation of these vesicles in the brain, accompanied by a significantly prolonged lifespan.
“Overall, EVs nanocarriers efficiently accumulate in lysosomes, which are the target organelles for delivery of the depleted lysosomal enzymes. This suggests that macrophage-derived EVs may be a promising drug delivery platform for the enzyme replacement therapy to treat different LSDs [lysosomal storage disorders],” the researchers concluded.