TPC2 Calcium Channel Could Be Therapeutic Target for Batten
A compound developed by researchers completely restored healthy waste deposit levels in cell cultures
Written by |
Activation of a type of channel called TPC2 may restore more normal lysosome function, offering a potential therapeutic approach for Batten disease and others marked by impairment of those cellular compartments, a study suggested.
When a cellular model of juvenile Batten disease was treated with a compound designed to activate TPC2 channels, lysosomes showed a restored ability to clear toxic protein buildup, a hallmark of Batten disease.
The study, “TPC2 rescues lysosomal storage in mucolipidosis type IV, Niemann–Pick type C1, and Batten disease,” was published in EMBO Molecular Medicine.
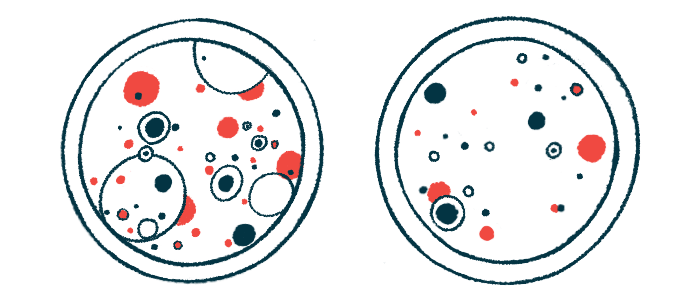
Lysosomal storage disorders are a large group of inherited diseases marked by the abnormal buildup of toxic materials in lysosomes, the cell compartments responsible for breaking down waste.
Batten disease is the collective name for a smaller group of lysosomal storage disorders caused by defects in the processes needed to break down lipofuscin, cellular waste deposits of fat and proteins, that accumulate in lysosomes. Nerve cells are particularly vulnerable to this buildup.
Normally, lysosomes release calcium to mediate cellular processes needed to clear waste. Disrupted calcium signaling in these cell compartments has been associated with multiple lysosomal storage disorders that affect the brain, including Batten.
An accumulating body of evidence has shown that activating certain channels involved in lysosomal calcium release could help restore more normal function in these diseases. In particular, researchers hypothesized that activating a channel called two-pore channel 2 (TPC2) may be beneficial, but the role of the channel has not been well explored.
To test their hypothesis, the researchers developed a compound called TPC2-A1-P, designed to activate TPC2, and tested its effects in cell cultures of fibroblasts — a type of connective tissue cell — from patients with juvenile Batten disease, or CLN3 disease, the most common Batten type.
Cells were first treated with mitomycin C, a compound intended to enhance lipofuscin buildup in lysosomes. TPC2-A1-P was able to completely restore lipofuscin levels comparable to those observed in cells from healthy people.
The treatment was also able to prevent accumulation of globotriaosylceramide (Gb3), another fatty protein that’s been shown to accumulate in CLN3 disease.
To expand their findings, the researchers used healthy human stem cells — cells that can become virtually any other cell type when treated in particular ways — to generate human-derived nerve cells in the lab. These nerve cells were genetically engineered to house a common mutation in the CLN3 gene that’s known to cause juvenile Batten. They also generated cells lacking CLN3 entirely.
Researchers observed that multiple channels known to be involved in lysosome signaling, namely, TRPML2, TRPML3, and TBC1, were undetectable in the mutated cells, while TPC2 was detected at levels similar to those seen in healthy control cells.
The diseased nerve cells also showed signs of an expanded lysosome compartment, reflecting toxic protein buildup.
Cells lacking CLN3 entirely also had low numbers of cristae in their mitochondria. Mitochondria are energy production centers that provide other cellular components, such as lysosomes, with the energy they need to function. They contain folds, or cristae, that increase their surface area and enhance their energy-producing capabilities. A reduced number of cristae reflects a reduced capacity for energy production.
Both lysosome expansion and cristae numbers were normalized with TPC2-A1-P treatment.
In mice, TPC2 was found to exist broadly across several brain regions, suggesting it could be a promising therapeutic target for lysosomal storage diseases such as Batten where the brain is most significantly affected.
Targeting TPC2 can restore more normal lysosome function in a cell model of juvenile Batten, and could represent a therapeutic target for the disease, the findings showed.
The study also identified beneficial effects of TPC2 activation in other neurodegenerative lysosomal storage diseases, including mucolipidosis type IV and Niemann–Pick type C1.
“Our results provide an incentive to further investigate the potential benefit of TPC2 activation in various [lysosomal storage diseases],” the researchers wrote.
TPC2-targeted treatments might also be beneficial for adult neurodegenerative diseases, where activating another lysosomal calcium channel, TRPML1, has shown benefits, the researchers noted.






