FDA Issues Guidance on Developing Rare Disease Treatments
Written by |

New guidelines from the U.S. Food and Drug Administration (FDA) may make it easier to develop therapies to treat extremely rare diseases, such as Batten disease.
“The release of this guidance from the FDA is a first step and a very welcome one. It speaks to the promise of precise, genetically targeted medicines for rare disease patients with currently unmet needs, and acknowledges the need for thoughtful frameworks to deliver on that promise,” Timothy Yu, MD, PhD, a physician at Boston Children’s Hospital and professor at Harvard Medical School, said in a news story.
In recent years, there have been substantial strides forward in the development of treatments for rare diseases. In the past eight years, the FDA has approved more than twice as many rare disease treatments as it did in the prior eight years.
In the case of genetic diseases, advancements in research have allowed clinicians to pinpoint the exact genetic cause of a disease — and, in some cases, to design therapies to specifically address the disease-causing mutations.
The first-ever such case occurred in 2017 when researchers at Boston Children’s Hospital developed a customized medication for a girl named Mila with CLN7 Batten disease. After the FDA gave its permission, Mila received the medication — called milasen — the next year, just nine months after her one-of-a-kind mutation was identified. One of Mila’s mutations (from her father) was a known Batten mutation, but the mutation from her mother could not be found.
The treatment substantially improved Mila’s condition, reducing the number and length of her seizures.
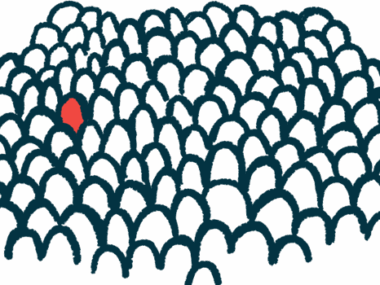
Mila’s case is an example of an “n of 1” therapy, meaning that the therapy was developed to treat a single individual. The FDA’s new guidance seeks to make it easier to develop such therapies.
The agency stated in a press release that doing this kind of treatment development, “brings a set of challenges and considerations not seen with the typical drug development process.”
For example, as was the case for Mila, the disease in these cases often progresses rapidly, so there is a need for fast medical intervention; that means the development of the medication needs to go very quickly.
Patients and their families also are more closely involved in the process than in traditional clinical trials, often functioning “more like drug development collaborators than traditional trial participants,” according to the FDA. As such, the agency has stressed the importance of giving patients and families all of the information they need to make an informed decision, including the possibility that an experimental treatment might not work, or might result in unforeseen side effects.
Another major difference from traditional drug development is that “n of 1” trials are usually led by academic centers, rather than by pharmaceutical companies, because there is little money to be made in developing medications that can treat only one or a handful of individuals.
“Academic medical centers are leading the way in creating customized treatments, since there are few commercial incentives to develop drugs for just a handful of patients,” said Yu, who helped to develop milasen.
The new FDA guidance aims to advise academic researchers — who may be less familiar with FDA regulations and policies — on how to go about interacting with the agency in the development of these medications. The guidelines also address issues like how to obtain informed consent from trial participants, and establishing appropriate ethical monitoring.
The guidelines focus specifically on a type of medication called antisense oligonucleotides (ASOs). These are short segments of artificial genetic code that mirror a particular piece of a patient’s DNA. Depending on their design, ASOs can turn genes “on” or “off,” or even increase the expression of a backup gene to achieve a therapeutic effect. Milasen is an example of an ASO.
Generally, ASOs have a good safety profile, and they are fairly easy to design and manufacture for personalized medicine; sequences of genetic code can be swapped in to address an individual patient’s mutation.
“Taking advantage of customized ASOs requires new ways of thinking about drug manufacture, validation, trial design, and approval,” Yu said.
Beyond Batten disease, Boston Children’s has launched “n of 1” clinical trials for two other diseases: ataxia-telangiectasia and KCNT1 epileptic encephalopathy. More trials are in the works.
“We are way out in front in creating a hospital process and structure for reviewing and monitoring these therapies” said David Williams, MD, chief scientific officer at Boston Children’s. “We have set up robust processes to ensure scientific rigor and patient safety, and to consider ethical questions. Other institutions are now emulating our example.”