Exome Sequencing is a Valuable Tool for Diagnosis of Pediatric Batten Disease
Written by |
Exome sequencing, a technique that looks for gene mutations, is a valuable tool to diagnose pediatric neuronal ceroid lipofuscinoses, also known as Batten disease, according to a new case report.
The study, “A novel MFSD8 mutation in a Russian patient with neuronal ceroid lipofuscinosis type 7: a case report,” was published in the journal BMC Medical Genetics.
Neuronal ceroid lipofuscinoses (NCLs) are a group of inherited lysosomal storage diseases caused by a lack of specific enzymes that break down certain fats or sugars in cells, leading to inappropriate storage of material in various tissues.
To date, researchers have identified more than 440 mutations related to NCL across 13 different genes.
Patients with NCL can be classified based on age at onset and clinical presentation: infantile, late infantile, juvenile, and adult.
Among patients with late infantile NCLs, several subtypes exist, including variant late infantile NCL (vLINCL). vLINCLs, for the most part, are caused by mutations in four genes — CLN5, CLN6, CLN7 (MFSD8), and CLN8.
Mutations in the MFSD8 gene, which provides instructions to produce a lysosomal protein, can give rise to a type of vLINCL called NCL7 disease.
NCL7 disease was first described in children from Turkey. This type of disease was considered a distinct clinical and genetic variant of NCL; however, subsequent studies have shown that NCL7 disease is not limited to the Turkish population.
In this case report, physicians presented a 5-year-old Russian girl with cognitive and motor deterioration, vision loss, action myoclonus (muscular jerking triggered or intensified by voluntary movement) and epilepsy.
The girl was developmentally healthy until she was 2 1/2 years old. After that, she experienced progressive motor and mental deterioration.
A brain magnetic resonance imaging (MRI) showed lesions in the white matter (the part of the brain responsible for carrying signals between neurons) and an underdeveloped lower cerebellar vermis (an area of the brain that integrates information from all our senses).
At age 3 1/2, the girl began developing stereotypic movements, which are repetitive and nonfunctional motor behaviors.
The child was treated with valproic acid — an antiepileptic therapy. But motor deterioration progressed and the patient stopped walking at age 5.
Based on observed symptoms, physicians suggested a diagnosis of Rett syndrome, a rare neurological disorder that results from mutation in a gene called MECP2. However, testing of the gene found it to be normal.
Several other diseases were also considered, but subsequently excluded based on mutations and biochemical tests.
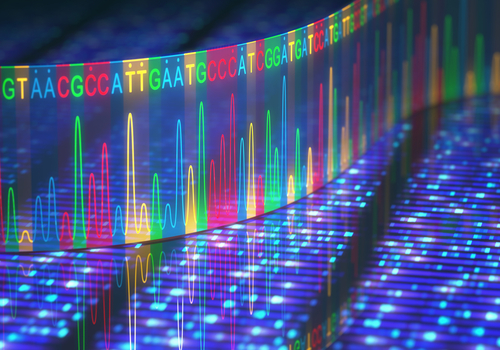
Physicians then conducted exome sequencing, which looks for mutations in all protein-coding genes of the genome — our genetic signature. It consists of two steps. The first selects only regions of the DNA that contain information that will result in proteins (known as exons, constituting only 1% of the human genome). The exons are then sequenced, or “read,” using specific DNA sequencing technology.
Exome sequencing revealed a particular type of mutation (c.525 T > A variant) in the MFSD8 gene. This specific mutation had never been previously described.
“This report describes the first case of NCL7 disease in Russia. Our findings expanded variant diversity of MFSD8 and proved value of exome sequencing for pediatric NCLs,” the authors wrote.
“Although there is no treatment for this condition, correct and early diagnosis is important for appropriate low-vision management, educational planning, and genetic counseling,” they concluded.