CLN2 gene therapy shows safety, promising efficacy in monkey study
AAVrh.10hCLN2 found better distributed when delivered into CSF of spine
Written by |
An experimental gene therapy for late infantile Batten disease showed a good safety profile and appeared to be working as designed in a study done in non-human primates.
“The advancement of this potential gene therapy could provide new hope to families with affected children,” Terence R. Flotte, MD, editor-in-chief of Human Gene Therapy, which published the study, said in a press release.
The study, “Assessment of Safety and Biodistribution of AAVrh.10hCLN2 Following Intracisternal Administration in Nonhuman Primates for the Treatment of CLN2 Batten Disease,” was funded in part by Lexeo Therapeutics, and led by a team including several scientists at the company.
Late infantile Batten disease caused by mutations in CLN2 gene
Late infantile Batten disease, also called Jansky-Bielschowsky disease or CLN2 disease, is caused by mutations in the gene CLN2, which provides instructions for making the protein tripeptidyl peptidase 1 (TPP-1). The TPP-1 protein is normally needed to break down molecular debris in nerve cells. Without a working version of the protein, the debris builds up to toxic levels, causing damage throughout the brain that gives rise to disease symptoms.
The gene therapy, referred to as AAVrh.10hCLN2, is designed to deliver a healthy version of the CLN2 gene into nerve cells, allowing the cells to produce a functional TPP-1 protein that can clear out toxic molecular debris.
It delivers its genetic payload using a specifically engineered virus called adeno-associated virus, which is commonly used as a vector for gene therapies because it’s good at getting genetic material into human cells, but doesn’t typically cause disease in people.
A preliminary Phase 1 clinical trial (NCT01161576) tested AAVrh.10hCLN2 in children with late infantile Batten disease, with the main goal of assessing safety. In that study, the gene therapy was administered via the intraparenchymal (IPC) route, with an injection through the skull directly into a specific part of the brain.
Results showed the treatment was generally well-tolerated, though abnormalities were seen on brain MRI scans of some patients. Neurological assessments suggested children treated with the gene therapy had slower disease progression than would be expected without treatment. However, the gene therapy did not stop disease progression.
The advancement of this potential gene therapy could provide new hope to families with affected children.
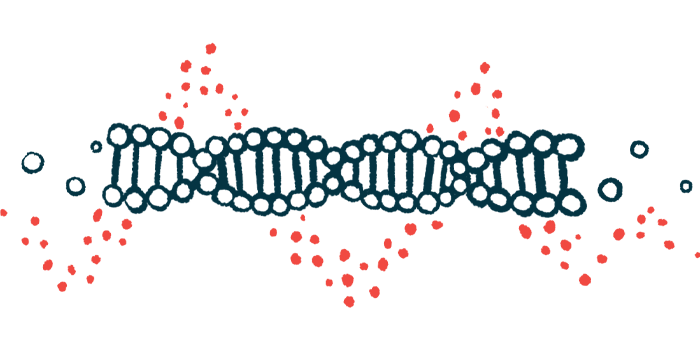
The less-than-perfect effect on disease progression likely means that, when delivered via the IPC route, the AAVrh.10hCLN2 gene therapy isn’t able to deliver its payload throughout the entire brain.
“While these initial clinical results were encouraging and safe, the IPC route of administration likely did not result in optimal distribution of AAVrh.10hCLN2 throughout the brain and the dose delivered did not result in sufficient TPP-1 expression to completely halt progression of the disease,” the researchers wrote.
In the new study, scientists conducted experiments in non-human primates (African green monkeys) to test a different form of administration called the intracisternal magna (ICM) route. In the ICM route, the gene therapy is injected into a pool of cerebrospinal fluid (CSF) that sits at the base of the spine. CSF is the liquid that surrounds the brain and spinal cord.
“Since the cerebrospinal fluid (CSF) bathes the entire [brain and spinal cord], delivery through the intracisternal magna (ICM) route should provide broad access to the brain, allowing higher doses with less safety/toxicity concerns than IPC delivery,” the researchers wrote.
The study included four monkeys: two were given a one-time dose of the gene therapy, and the other two were given an inactive saltwater solution as a control.
Researchers study potential safety issues with ICM delivery of gene therapy
The main goal of these experiments was to look for any unexpected safety issues associated with ICM delivery of AAVrh.10hCLN2. The researchers conducted detailed analyses including looking at the monkey’s behavior, scans of their brains, and lab tests of bodily fluid and tissue from organs. Across all these assessments, results broadly showed no noteworthy safety problems linked with the gene therapy.
Analyses also indicated monkeys treated with gene therapy had an increase in TPP-1 in their CSF, with levels rising to roughly half those seen in healthy people. Of note, TPP-1 levels as low as 10% of normal are expected to provide a therapeutic benefit in Batten disease.
Brain analyses also showed the gene therapy was widely distributed. Most analyzed areas of brain tissue showed substantial levels of TPP-1 protein, and the protein’s expression in the brain was overall higher than in earlier preclinical studies that used the IPC route of administration.
“Collectively, the safety data and the vector and protein distribution data demonstrate that AAVrh.10hCLN2 delivered by ICM administration is safe and leads to wide, likely therapeutic brain and CSF distribution of TPP-1,” the scientists concluded.