CellCept Safe, But Ineffective, in Phase 2 Study for CLN3 Disease
Roche’s CellCept was safe, but lacked clinical benefits, during short-term use by patients with CLN3 disease, according to the results of a Phase 2 clinical trial.
The study, “Short-Term Administration of Mycophenolate Is Well-Tolerated in CLN3 Disease (Juvenile Neuronal Ceroid Lipofuscinosis,” was published in JIMD Reports.
CLN3 disease, or juvenile neuronal ceroid lipofuscinosis, is a rare, inherited lysosomal storage disorder caused by mutations in the CLN3 gene on chromosome 16. At 4-6 years of age, affected individuals develop blindness, followed by developmental regression that includes cognitive and motor decline and epilepsy.
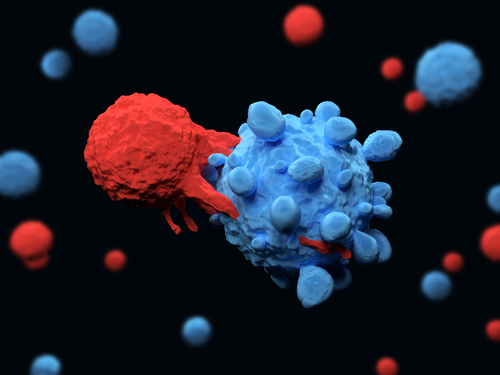
Preclinical and clinical data suggest that autoimmunity — when the immune system attacks the body’s own tissues — and inflammation in the brain contribute to neurodegeneration in patients with CLN3 disease. For instance, autoantibodies against brain proteins can be found in the blood of patients with CLN3 disease.
Researchers are studying the use of immunosuppressive agents (those that suppress the immune system and the production of autoantibodies) to treat CLN3 disease and other neuronal ceroid lipofuscinosis.
Cellcept (mycophenolate mofetil), an immunosuppressant approved by the FDA to prevent organ transplant rejection in children, is commonly used off-label to treat pediatric neurological conditions linked with the immune system.
Following positive preclinical data in mouse models of CLN3 disease, where Cellcept reduced nerve cell death and reverted motor problems, a Phase 2 clinical trial (NCT01399047) evaluated the safety and tolerability of CellCept in CLN3 patients.
The double-blind, crossover study examined the safety of short-term (eight weeks) administration of CellCept versus placebo in ambulatory children with CLN3 disease.
A total of 19 patients, mean age 12.5, were randomized to receive eight weeks of CellCept followed by eight weeks of placebo with a four-week “washout” interval, or vice versa. Total study time was 22 weeks.
Participants were given an oral liquid formulation of CellCept, starting at half the target dose, during the first two weeks, then increased to the full dose (600 mg/m2/dose), twice daily up to a maximum of 1,000 mg twice per day.
Patients and caregivers were consulted at baseline, and at weeks 8, 12, and 20. In addition, disease outcomes were measured using clinician-reported assessments and a battery of tests to address patients’ motor features, seizures, behavior, cognitive and functional measures.
CellCept was well-tolerated, with nearly all patients (89.5%) coping well with the medicine and completing the study. In fact, there were no significant differences in tolerability rates between CellCept and placebo groups.
No serious side effects were observed. All reported events were also present in the placebo group and mild. The most common were vomiting (31.6%), diarrhea (15.8%), and cough (15.8%).
However, there were no definite effects on measured autoimmunity or clinical outcomes in the setting of short-term use of CellCept.
The brief exposure to treatment was useful to study short-term safety risks and support future long-term studies, but it “did not allow clinical insights into potential efficacy,” researchers stated.
“Long-term administration of mycophenolate in individuals with CLN3 disease is needed to determine whether there is a disease-modifying clinical benefit and whether it is safe for long-term use in this fatal neurodegenerative condition,” they concluded.





