CLN2 Mouse Model Shows Small Vesicles May Help Deliver TPP1 to Brain
Small vesicles naturally produced by certain types of immune cells may be used as carriers to deliver TPP1 — the enzyme missing in patients with late infantile Batten disease — to the brain, a mouse study has found.
If implemented in future therapies, this strategy could allow for more effective treatment of patients, using lower treatment dosages and less invasive modes of administration, the researchers noted.
The study, “Extracellular Vesicles as Drug Carriers for Enzyme Replacement Therapy to Treat CLN2 Batten Disease: Optimization of Drug Administration Routes,” was published in the journal Cells.
Late infantile Batten disease, also known as CLN2 disease, is a rare neurodegenerative disorder caused by genetic mutations in the TPP1 gene, which provides instructions for making an enzyme called tripeptidyl peptidase 1 (TPP1).
This enzyme normally found in lysosomes — small cell compartments that digest and recycle different types of molecules — is responsible for breaking down proteins that are no longer needed. However, when TPP1 malfunctions, these proteins start to build up inside cells, reaching toxic levels and leading to the onset of disease.
One of the major hurdles in the development of new therapies to alleviate the neurological symptoms of CLN2 disease is the delivery of functional TPP1 to the brain, which is separated from the rest of the body by a highly selective semipermeable membrane called the blood-brain barrier.
“Recently, the first FDA-approved treatment [for CLN2 disease], [brain] infusions of a recombinant [man-made] form of human TPP1, Brineura, was shown to provide symptomatic improvements in pediatric patients. Unfortunately, this invasive procedure carries a high risk of adverse effects,” the researchers wrote.
Brineura (cerliponase alfa) is infused directly into the fluid surrounding a patient’s brain, a method known as intraventricular infusion.
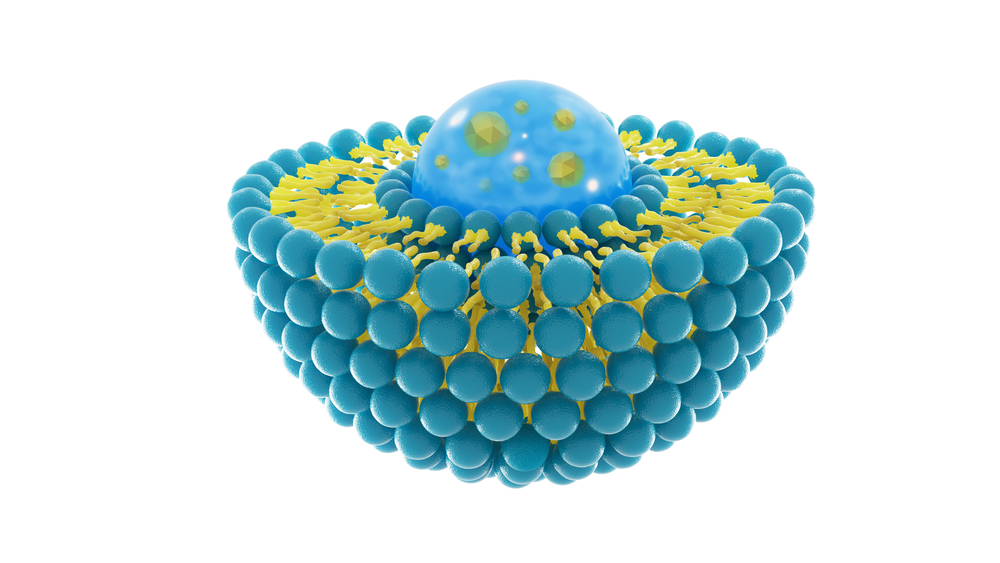
Researchers at the University of North Carolina at Chapel Hill have now attempted a less invasive method to transport and deliver TPP1 to the brain: small extracellular vesicles (EVs) naturally produced by macrophages — immune cells that are responsible for removing debris and dead cells from tissues.
EVs are small membrane particles that contain different types of molecules that can be exchanged between cells. These small vesicles can be released by different types of cells, and are usually found circulating in the plasma or other types of body fluids.
“We previously demonstrated that macrophage-derived EVs home to regions of inflammation and neurodegeneration accumulate at therapeutically relevant amounts, and deliver therapeutic proteins to the [central nervous system],” the researchers wrote.
To investigate the viability of this therapeutic strategy, they administered macrophage EVs containing functional TPP1 (EV-TPP1) to a mouse model of CLN2 disease, using four different modes of administration: intranasal (through the nose); intravenous (into the vein); intraperitoneal (through the abdominal cavity); and intrathecal (through the spinal cord) injections.
After that, they examined the distribution and documented the efficacy of EV-TPP1 in each case.
Intrathecal and intranasal administration of EV-TPP1 led to a high accumulation of TPP1 in several areas of the brain, particularly the hypothalamus and thalamus. This was also accompanied by a reduction in neurodegeneration, brain inflammation, and buildup of toxic substances inside lysosomes.
Intravenous and intraperitoneal administration of EV-TPP1 resulted in the delivery of TPP1 to other organs, including the liver, kidneys, spleen, and lungs.
A combination of intrathecal and intraperitoneal administration of EV-TPP1 significantly prolonged animals’ lifespan, compared with animals treated with a saline solution or TPP1 alone.
“The ultimate goal of our investigations is to develop a next-generation Brineura product using natural nanocarriers, EVs. From a clinical perspective, the benefits could include reduced dosage and administration through different and less invasive routes, … [improved] therapeutic efficacy and decreased offsite toxicity,” the researchers wrote.
“We suggest that different regimens using EVs-based formulations of TPP1 should be considered according to the age of patients, the disease progression, and [disease] manifestations,” they added.





