Common Batten Tests Spot Biomarkers in Mouse Model That Track Progression
Written by |
Common, non-invasive imaging techniques and a walking test used to assess patients with Batten disease in the clinic helped scientists identify a new set of biomarkers in a mouse model that can track disease progression over time, a study reports.
These findings support the accurate translation of results from preclinical animal studies to human clinical trials, which is critical to developing new therapies.
The study, “A multimodal approach to identify clinically relevant biomarkers to comprehensively monitor disease progression in a mouse model of pediatric neurodegenerative disease,” was published in the journal Progress in Neurobiology.
The increasing pace of work in Batten means more potential medicines are moving from preclinical studies in animals to clinical trials involving people.
As such, there is a need for accurate biomarkers of use both in animal models and in people, and that are minimally invasive and can be monitored over time, especially in childhood disorders like Batten. Because neurodegeneration can occur months before obvious changes in behavior, biomarkers are also essential for early disease detection.
An animal model called the Cln6-nclf mouse is used to support the research into a variant form of late infantile Batten disease, in which patients carry a mutation in the CLN6 gene. This model has been shown to capture many hallmarks of the human disease, both clinically and behaviorally.
However, many tests rely on mouse-specific behaviors, and disease or treatment analysis is often conducted post-mortem.
Researchers at the University of South Dakota investigated the Cln6-nclf mouse to find biomarkers for Batten disease using noninvasive methods that can be followed over time — and better translate to clinical practices with patients.
As studies have failed to find a single biomarker to follow Batten progression, the research team examined these mice using four non-invasive imaging techniques and a walking (gait) test — all commonly used in assessing patients.
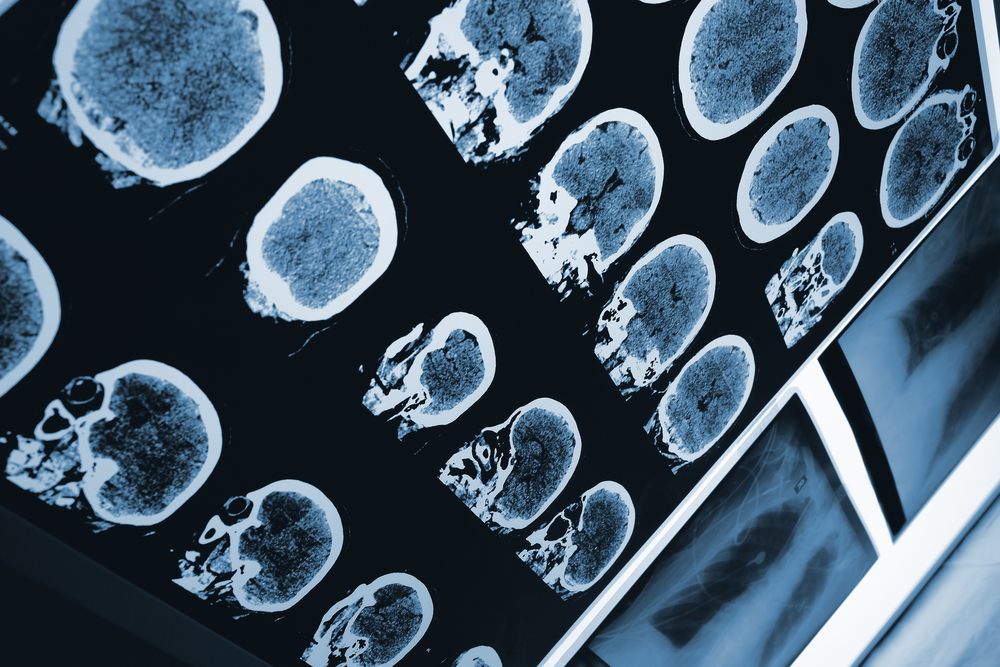
The brains of Cln6-nclf mutant mice, along with normal mice, were examined between 3 and 12 months of age using two MRI techniques that capture brain structure and tissue damage, and magnetic resonance spectroscopy (MRS) and positron emission tomography (PET) to measure metabolic changes.
Between 6 and 12 months of age, the mice’s motor skills were tested using a kinematic gait analysis, which measures a number of walking characteristics.
MRIs to detect changes in brain structure found that, overall, the whole brain volume of the Cln6-nclf mutant mice decreased over time compared to normal mice, reaching significance at age 9 months. At 3 months old, significant volume decreases were found in the hippocampus — the brain region associated primarily with memory.
Nerve cell degeneration (atrophy) was observed to reach about 14% at age 9 months in the cortex, the outer layer of the brain that plays a role in processes such as perception, thought, language, and consciousness. Also reduced in size were areas responsible for movement, called the striatum and the cerebellum.
Changes were seen in both the outside grey matter, which is made of neuron cell bodies, and the inside white matter, which consists of signal-sending axons that form connections between brain cells.
MRS analysis found changes in a variety of metabolites at various time points, including a steady drop in a metabolite called N-acetylaspartate (NAA). The NAA decrease in these mice mirrored what is seen in Batten patients.
Using PET for more detailed metabolic assessment revealed changes in nerve cell metabolism, the uptake of glucose for energy, and inflammation.
Kinematic gait analysis examined the walk cycle, body and head orientation, and other factors related to the limbs. Results found that the Cln6-nclf mutant mice had progressive walking disturbances that mirrored those described in CLN6 disease patients.
Finally, the team conducted a type of analysis aimed at identifying a core set of disease characteristics that strongly correlate with one another to best describe disease progression.
Altogether, the best measures were a decrease in brain volume associated with poorer overall mobility; metabolic changes in areas such as the striatum, grey matter, and cerebellum; and changes to white matter.
“This innovative, highly sensitive platform can be used as a powerful tool for preclinical studies on neurodegenerative diseases, and provides proof-of-principle for use as a potentially translatable tool for clinicians in the future,” the scientists concluded.